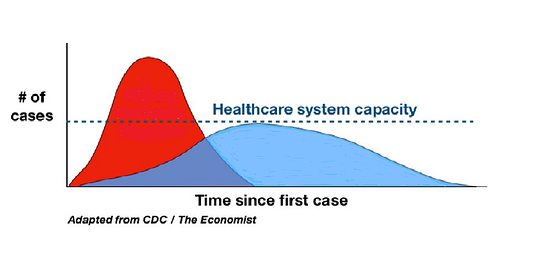
More than half of U.S. states have instituted lockdown measures in response to the spread of the COVID-19 virus. These policies are justified as an effort to “flatten the curve,” a phrase coined by Dr. Howard Markel, a pediatrician, and professor of medical history at the University of Michigan.
The hypothetical COVID curve we are trying to flatten — the time rate at which the number of people needing intensive medical treatment will grow to exceed our capacity to care for them — is based on assumptions about when COVID was brought to the US, the speed of its transmission, and the ability of our healthcare system to accommodate the most severely affected patients. By isolating citizens in their homes, lockdown policies intend to slow the rate of infection, thereby “flattening” the curve, which will allow us to ration healthcare resources over time.
“Flatten the curve!” has become the rallying cry of politicians, public health officials, celebrities, and social media users who believe that, without extreme social distancing measures, the American healthcare system will invariably be overwhelmed resulting in several million unnecessary deaths. The theory goes that if we succeed in flattening the curve, millions of lives will be saved.
It’s important to remember that a flat curve is not one in which no one gets infected. A flat curve is one which, at its peak, does not create enough critically ill patients to overwhelm the health care system.
The model with the most profound impact on public health policy was produced at Imperial College on 16 March 2020. It compared the health outcomes of suppression (i.e., lockdown) with less restrictive policies and predicted that millions in the United States and United Kingdom (2.2 million and 500K respectively) would die from COVID-19 unless aggressive containment measures were instituted immediately.
Since publication, new data has challenged the Imperial College model. Points of contention have centered around hospitalization, fatality, and transmission rates. The lead author of the study has since revised the fatality expectations substantially downward. So there are some adjustments being made to the initial assumptions.
But there’s one data point being used in all of the prevailing models, including Imperial, that no one is talking about.
When did the COVID curve begin?
And it’s an important point. How can we interpret the data we currently have if we don’t know where on the time axis we actually are?
Starting the Curve
“Seed date” is a term used in pandemic epidemiology to identify when a disease was first established in a specific location. Knowing that date, or at least an approximate range, allows scientists and data modelers to calculate how far the disease has spread, how fast it’s spreading, and use that information to design effective responses.
Determining when a disease originated and implementing effective test-track-isolate protocols is critical to the effective management of infectious diseases. Suppression is a far easier process when you have the cooperation of governments and health authorities who value transparency and knowledge-sharing. Management becomes much tougher when you are confronted with a virus, especially one that spreads as silently as COVID, whose country of origin attempted to hide its existence.
When the Imperial College model relied on Chinese data about the origins of COVID-19 and presumed that COVID was seeded in the United States in early January, they were likely predicating their output on flawed input.
Because the first confirmed case of COVID in the United States was identified 20 January in Washington State, setting the seed date a week or two earlier must have seemed reasonable.
It is not.
China went to great lengths to hide the existence of COVID by censoring communication about the disease and ordering lab samples destroyed. Two Chinese journalists covering the COVID outbreak, Chen Quishi and Li Zehua, have gone missing. They lost control of the narrative on 30 December when two physicians, Ai Fen and Li Wenliang — one of whom has died and the other who has since disappeared — attempted the day before to warn colleagues of cases of “SARS” at their local hospital.
China then reported an ”unknown pneumonia” to the WHO on 31 December, and on the same day claimed they had not found evidence of human-to-human transmission.
According to Straits Times,
Around that time,[27 Dec 2019] doctors sent at least eight other patient samples from hospitals around Wuhan to multiple Chinese genomics companies, including industry heavyweight BGI, as they worked to determine what was behind a growing number of cases of unexplained respiratory disease. The results all pointed to a dangerous Sars-like virus.
That was days before China notified the World Health Organisation (WHO) on Dec 31 about the emergence of an unidentified infectious disease, two weeks before it shared the virus’ genome sequence with the world, and crucially, more than three weeks before Chinese authorities confirmed publicly that the virus was spreading between people.
During (and likely before) that time, asymptomatic carriers were rapidly spreading the virus throughout one of the most densely-populated, internationally-connected cities in the world and beyond.
China did not release the RNA sequence required to create a COVID test until 12 Jan. The virus had already spread so far by that time that the first confirmed case outside China was discovered in Thailand the very next day.
Two months elapsed between the date China claims COVID originated and when the test sequence was made available in January. That means there were at least 60 days of undocumented spread of a highly transmissible, often asymptomatic virus. COVID could’ve seeded itself all over the world and spread undetected for several months and no one in the US could’ve even tested because there was no available test until the very end of February. And even then, neither the test nor the components needed to run the test were readily accessible.
Without reliable data from a reliable source, we can only estimate the seed date using what we know.
So then the question becomes, what do we know?
A Mysterious Flu-like Illness Arrived in the US In Nov 2019
Stating that COVID is “just a flu” has become a notorious trigger for outrage on social media sites. Statistics and debates about varying characteristics and severity inevitably ensue, but the comparison is the product of the indistinguishable overlap in their respective symptoms.

In December 2019, the UK’s National Health Service (NHS) reported that they were experiencing an exceptionally bad flu season and conducted media outreach to encourage citizens to get their flu shots in hopes the campaign might curtail the outbreak.
Almost 12,000 patients across Britain went to their GP last week (Dec 9 -15) complaining of influenza-like symptoms, such as a fever, aching muscles and headaches.
This is 25 per cent higher than the week before, where 9,500 — including almost 8,000 from England — sought advice for similar symptoms.
On top of the soaring GP visits, there were more than 50,000 calls made to NHS 111 regarding cold and flu.
An early start to the season has left 2,092 people in England needing treatment for the contagious virus so far in 2019. By comparison, there were just 256 hospital admissions with flu at the same point 12 months ago.
And the number of patients rushed into intensive care with the flu is three times higher than last winter.
Many of those calls, doctor visits, and hospitalizations categorized as “flu-like-illness” may have been due to the novel coronavirus for which the UK did not know to be looking and was not able to test and, ergo, assumed that it was “just the flu”.
Especially given the surprising degree of illness severity noted in the article.
Because many of COVID’s symptoms are so similar to the flu, a good place to look for indications of COVID’s early presence in the US is in the CDC Flu Surveillance data. If COVID were widely disseminated in November or December, it’s presence would have likely caused an increase in doctor visits shortly after it began its rapid spread.
Here is a graph of weekly physician-reported visits for Influenza-like-illness (ILI) reported to the CDC for 2019–2020 year-to-date and for the last two flu seasons.
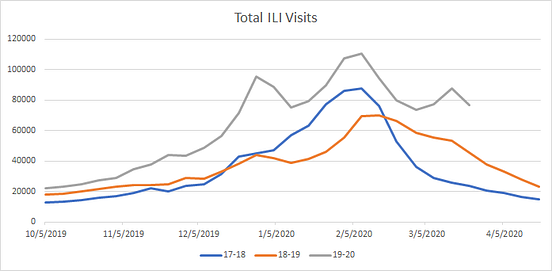
Nearly twice as many ILI visits were reported during the beginning of the 2019–2020 flu season than were reported in either of the two previous years. By December 2019, there were over 80,000 US patients seeking treatment for flu-like symptoms — long before Chinese authorities reported COVID to global health organizations on 31 Dec 2019.
Many of the Americans reporting flu symptoms had one of the six strains of ordinary, seasonal flu routinely monitored by the CDC. However, those cases do not account for either the timing nor the dramatic increase in ILI this year. The graph below shows how the volume of positive seasonal flu tests per week in 2019–20 compares to previous years.
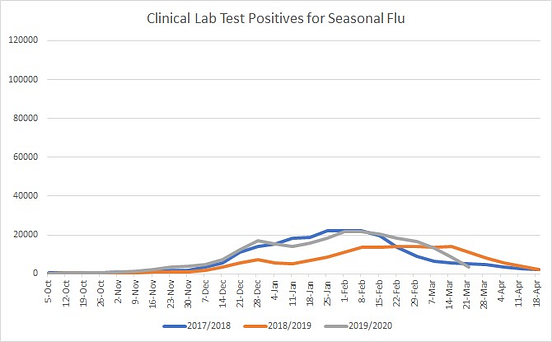
The number of positive seasonal flu tests is relatively small in comparison to total ILI visits. That is, most cases of ILI visits in any given year remain unexplained by the flu. However, this year was unique in both the sheer volume of unexplained ILI visits and the early date that the surge of visits began.
Even 2017–18, the most deadly flu season in four decades, did not produce either the volume or the extended duration of ILI visits that year that we have seen over the past 6 months.
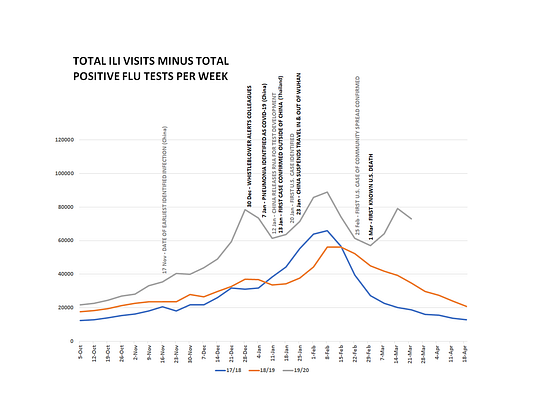
Subtracting the weekly positive seasonal flu tests from the total number of ILI visits for each year reveals that in late 2019, tens of thousands of Americans per week were complaining of a mysterious, unidentified illness that acts enough like the flu to be included in flu surveillance data.
The unidentifiable, mysterious flu-like illness curve looks like this:
A simple explanation for the dramatic increase in ILI visits in November-December 2019 is an earlier-than-presumed seeding of COVID in the U.S.
Taking into account CDC Flu surveillance data, the early-January seed date utilized by the Imperial Study seems unlikely.
Covert COVID
There is additional anecdotal, deductive, and empirical evidence which, in conjunction with the flu surveillance data, supports the theory that COVID was established in the US well before the first confirmed case.
For example, in my own story, I describe how and why I believe my family already had COVID-19 in January and February. The symptoms we exhibited were specific enough to warrant the assumption of COVID infection under current CDC guidelines.
And we’re not the only ones.
If we allow for an earlier seed date, hundreds of thousands of flu-like illnesses that occurred in the months before the first officially recognized US case can also retrospectively be characterized as COVID, based on their symptoms alone.
When we don’t know what we are looking for and we don’t question assumptions, information that might otherwise seem obvious can go unnoticed.
But when we do look for evidence, it’s not difficult to find. And as antibody tests become available, there will be more and more data about who has already been infected.
Why this matters so much.
A better understanding of where the COVID curve begins will improve anticipation and rationing of healthcare resources — both among COVID cases and for people with non-COVID related illnesses who are in need of medical care.
The path forward for COVID, US healthcare, and the global economy is very different when you assume November 2019 was the beginning of the pandemic.
Shifting the COVID 60 days back in time means the impending peak that everyone fears 60 days from now may be happening in real-time.
It means that we are grossly overestimating the case fatality rate and that what we fear is just the beginning may actually be the peak.
It’s possible that the COVID curve is already flat because if we are at or nearing the peak, we are effectively coping with the healthcare demand, and a large segment of the US population may already be immune, rendering most, if not all, of the impending economic damage unnecessary.
If COVID began 60 days earlier, canceling “elective” healthcare procedures, closing schools, and shutting down the economy is too high a price to pay to slow the rate of transmission of a disease that is slowing on its own and has a much lower case fatality rate (CFR) than initially assumed.
I will admit that I have a horse in this race. Five of them, actually. I’m one of the millions of people paying that very high price.
Fifteen months ago, I was diagnosed with a tumor in my liver. Because of its location, the risk/benefit of performing a diagnostic biopsy on the mass was too low to justify proceeding, so my oncologist took a watch-and-wait approach. Six months ago, I was relieved by a follow-up scan that indicated it had not grown. Nonetheless, in the last two weeks, I have developed GI symptoms that are consistent with the tumor spreading. As of now, I am unable to get a scan to rule out the possibility of metastasis of my disease because the imaging necessary to monitor my liver is considered “elective”. And when the healthcare system does finally come back online, the backlog of patients like me will result in even more delays to access.
Should the worst-case come to pass for me, and I later discover that I do have cancer that has spread and we missed the window to diagnose and treat it, my life will be one of many casualties of the COVID response. My four daughters will grow up without their mother and will likely be left in the custody of their father whom they currently only see every other weekend (two of them are completely estranged for him) and who has recently lost his job as nurse administrator of an outpatient orthopedic surgical facility due to CVOID-19. The owners were forced to shut the facility down a week ago because the governor of our state issued a ban on elective surgeries. His financial stability is doubly in question because the economic security measures that have been put in place for individuals affected by COVID specifically exclude healthcare workers.
So, in my little family alone, not only are my kids suffering the typical cabin fever and educational setbacks, but I have lost most of my freelance writing income, their father has lost his job which provided 50% of our financial support, we were not able to pay rent yesterday, and I am unable to obtain what could potentially be life-saving health care.
The current cumulative total of hospitalized COVID patients in my home state of Arizona as of this writing, and for which all of these sacrifices are being made, is 228. And that’s the cumulative number than has been accruing since March 24th, not the number currently hospitalized. Arizona has 14,790 hospital beds.
Our curve is flat.
My family is making mandated sacrifices in order to reserve capacity in the healthcare system for COVID patients who do not currently (and likely will never) exist — all because the COVID curve predicated on an inaccurate seed date says that the overwhelming surge is just barely beginning.
And our circumstances are not special.
Just in the realm of “elective” healthcare, melanomas across the nation are metastasizing because routine mole checks aren’t being conducted. Cancers are growing unrestricted because hospitals aren’t allowed to do most surgeries. Early diabetes is going undiagnosed because you can’t do A1C bloodwork with closed labs. Both life-saving and quality-of-life-preserving care is being withheld because we are conserving capacity for COVID-19 patients that, in a lot of areas, will never materialize.
And, health-related considerations aside, we are also wrecking the livelihoods of millions of Americans in service of preventing transmission among many who have likely already been exposed and recovered.
Ten million Americans filed for unemployment in the month of March. Small businesses are being forced to choose between closing their doors and incurring crippling long-term debt. The economy is teetering on collapse. Careers are being demolished. Retirement savings are vanishing. Children are trapped in abusive homes and domestic violence reports are sky-rocketing all because — in our panic — we never critically questioned when the COVID curve really began.
This is not who we are
We have a chance to gather more information and stop this. We have information at our fingertips that could help us pinpoint exactly where we are on the curve, determine an accurate case fatality rate, and tailor less draconian mitigation measures specific to each geographic locale. We have the ability to tailor responses to specific areas and support communities hardest hit by the surge, like NYC and Louisiana.
The U.S. just approved a test for COVID antibodies. According to the New York Times,
People with immunity might be able to venture safely from their homes and help shore up the work force. It may be particularly important for doctors and nurses to know whether they have antibodies.
Antibody testing eventually should give scientists a better sense of how widespread the infection is in the population and help researchers calculate more precisely the fatality rate and the frequency of asymptomatic infections.
What will it take for antibody testing to become a priority for US health officials? What happens when we look at the COVID response devastation in the rearview mirror and say, “That didn’t have to happen after all.”?
I hope I’m here to see it.
The possibility that we may be 60 days in time from where we have been told we are should be good news. The idea that right now may be as bad as it’s going to get should be elating. We should be clamoring to determine the least-restrictive, most-effective way to manage this novel outbreak.
But I know that there’s a difference between “shoulds” and what actually is. We have been too busy shaming our neighbors for getting fresh air and hoarding toilet paper to consider that we are being driven by fear, not fact and that it has shut down our ability to recognize inconsistencies and look for answers. Instead, we call anyone who questions the “sky is falling” narrative selfish, stupid, and irresponsible because aligning with the prevailing moral outrage renders us impervious to criticism.
And I don’t recognize us. That is not who we are.
We are Americans. We are innovative, resourceful, diverse, and dynamic. We are capable of addressing both the lethality of COVID and our economic stability. We are capable of protecting the sick and the vulnerable without requiring the world to come to a standstill with no idea how to restart it.
The most valuable tool we need in order to perform metaphorical surgery on this outbreak is accurate information. And to get that information, we have to be open to the idea that some of our fundamental assumptions about COVID-19 are wrong.
- Thomas P Seager, PhD contributed to this story.
Additional suggested reading:
- My experience with possible COVID:
I’m Convinced That My Family Already Had COVID-19.
Here is our story and a timeline, told via text.
medium.com
- How COVID silently spreads: Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV2)
https://science.sciencemag.org/content/early/2020/03/24/science.abb3221 - How antibody testing will help us understand where on the curve we are: Fundamental principles of epidemic spread highlight the immediate need for large-scale serological surveys to assess the stage of the SARS-CoV-2 epidemic https://www.medrxiv.org/content/10.1101/2020.03.24.20042291v1
- Why COVID behaves so differently in different locations: http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.138.1721&rep=rep1&type=pdf
- Why getting sunshine and being outdoors is good for your immune system: https://www.morozkoforge.com/post/prevent-coronavirus-covid-19

Written by